Introduction
Every summer, as the weather warms and the pools fill, community pharmacists start to see patients experiencing ear pain, often after swimming. The culprit is often acute otitis externa — otherwise known as swimmer’s ear— a painful, itchy inflammation of the ear canal which thrives on humidity and water.
For pharmacists, these are moments to demonstrate the evolving role of pharmacy practice: combining clinical skill, patient trust and timely education to deliver real relief. Even in jurisdictions where pharmacists can’t yet prescribe, their accessibility and expertise make them the logical first stop for early assessment, self-care advice and safe referral.
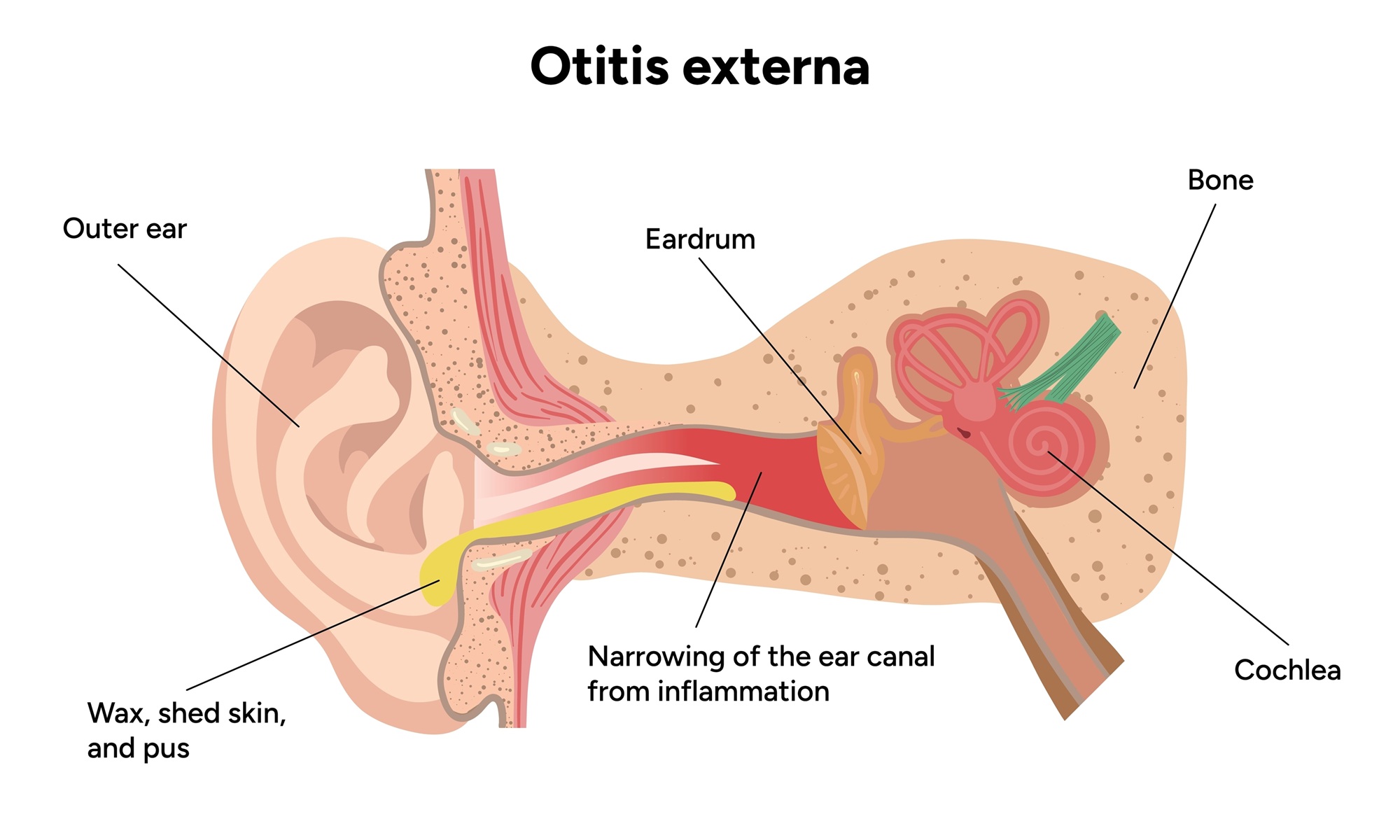
Otitis externa (OE) is an inflammation of the external auditory canal, most commonly caused by Pseudomonas aeruginosa or Staphylococcus aureus1. Fungal infection occurs less often but is more common in humid conditions or after prolonged use of antibacterial drops2. It can affect anyone, but the highest rates are seen among children and adolescents who spend hours in the water3.
The pathophysiology is uncomplicated and helpful to explain to patients: the ear canal is thin, delicate skin, protected by a slightly acidic layer of cerumen or wax. When moisture, trauma from cotton buds or earbuds, or prolonged use of hearing aids disrupt this barrier, the environment becomes perfect for bacterial growth4. Within 48 hours, inflammation, swelling and pain appear.
The environment a person lives, works and plays in can make all the difference when it comes to ear health. Warm, humid climates create ideal conditions for bacterial and fungal proliferation, and recreational habits such as daily swimming, surfing, or prolonged headphone or hearing-aid use can trap moisture and reduce ventilation. Behavioural factors contribute just as strongly, where vigorous ear cleaning utilising cotton buds or hairpins, strips away the protective wax barrier and causes micro-abrasions that allow pathogens to enter.
Even hair products or sprays that reach the ear canal can change its pH and natural microbiome balance. Patients with eczema, psoriasis or seborrhoeic dermatitis affecting the outer ear are especially prone, as are those with diabetes, whose reduced immunity and slower wound healing can turn a minor irritation into infection.
Patients usually describe sharp or throbbing pain, sometimes severe enough to disturb sleep. Itching, discharge, a sense of fullness and mild hearing loss are common. Pain on pulling the pinna or pressing the tragus is a classic sign5.
Clinical presentation and diagnosis
While it’s tempting to leap straight to treatment, managing OE safely in a pharmacy starts with a thoughtful consultation. The quality of history taking, examination and reasoning directly affects whether the patient walks away with the right advice.
A good consultation begins with listening to the patient. Pharmacists should invite patients to tell their story: What has brought you in today? When did this start? Is it affecting one or both ears? Have you experienced this before? Can you describe the pain or discomfort? Is there pain anywhere else? Have you been unwell?
Exploring triggers like swimming, humidity, dust exposure, vigorous ear cleaning or device use provides valuable clues. Ask about fever, diabetes, immune compromise, trauma, hearing loss, any prior ear surgery or grommets, and recent antibiotic or antifungal therapy.
Clarify what the patient has already tried, such as cotton buds, over-the-counter drops or home remedies. Always enquire if these treatments have been helpful, if the patient has noticed any improvement, or if their symptoms have worsened7.
Observing how patients describe their discomfort can also be diagnostic. If they point to pain in front of or behind the ear, think of mastoiditis or otitis media; if they focus on itch and fullness, it’s likely local canal inflammation.
Physical examination
Once a comprehensive history has been considered, a physical examination can confirm or refute probability diagnoses. For pharmacists who have appropriate training, the examination should start with a general inspection of the patient and measurement of relevant vital signs followed by inspection of the eyes, nose and mouth and palpation of lymph nodes and the temporomandibular joint.
Consider, sinus palpation if relevant. Following this, examine the outer ear for lesions, scars, redness or swelling, and press gently on the tragus, where sharp pain reinforces an Otitis Externa diagnosis7. Inspect behind the ear for tenderness or swelling, which may suggest infection spread or mastoiditis.
The purpose of otoscopic examination is to evaluate the condition of the ear canal, tympanic membrane and the middle ear. An otoscope is a tool which shines a beam of light to help visualise and examine the condition of the ear canal and eardrum. Otoscopy, should start with the less painful ear. Note canal redness, oedema, debris or discharge. Identifying visible redness, swelling, or discharge supports the suspicion of otitis externa. A clear, pearly tympanic membrane is reassuring, but if the view is obscured or the patient cannot tolerate the exam, provide analgesia and refer rather than persist9. If concerned about hearing loss, a whisper test can be conducted.
From there, clinical reasoning ties the findings together. Acute otitis externa can generally be diagnosed when three things line up:
- A rapid onset (within 48 hours),
- Ear pain worsened by manipulation, and
- Visible inflammation of the canal10.
The key question for pharmacists is not just “What is it?” but “Is it safe for me to manage?”
Red flags such as complete canal occlusion, spreading redness, systemic symptoms like fever or malaise, diabetes, immunosuppression, or suspected medium to large perforation of the tympanic membrane mean referral is essential11.
Differential diagnosis supports sound clinical reasoning. Deep ear pain with fever and a bulging tympanic membrane point toward acute otitis media. Recurrent itching and scaling may reflect chronic OE or seborrhoeic dermatitis. Fluffy white or black debris with intense itch suggests fungal OE.
Persistent severe pain out of proportion to examination findings, especially in someone with diabetes, raises concern for necrotising OE which is a medical emergency12. Recognising these patterns helps pharmacists triage confidently and practice safely.
Even without formal prescribing or extended-scope training, pharmacists can still conduct a safe, structured visual and symptom-based assessment that provides valuable diagnostic clues. Start with careful observation. Simply looking at the ear, rather than into it, can reveal a lot.
Check for swelling, redness or crusting around the outer canal, and ask the patient to gently move their pinna. Sharp pain on movement is a hallmark of acute otitis externa8. If otitis externa is suspected, the patient should be referred to a practitioner who can adequately assess and treat their condition.
Treatment options and product recommendations
Once serious causes are excluded, management becomes straightforward and highly effective.
For uncomplicated OE, the priorities are to keep the ear dry, control pain and apply appropriate topical therapy13.
AOE can affect people of any age but is more common in children and adolescents aged between five and 14 years. The treatment of children with otitis externa is no different to adults as long as safety of the prescribed ear drops is confirmed for the child’s age. In Queensland, where trained pharmacists are currently able to assess and treat otitis externa, eligibility criteria excludes children aged younger than two years from pharmacist care.
Non-pharmacological advice is simple but powerful. Patients should avoid swimming and keep the affected ear dry until fully healed. During showers, a silicone plug or cotton ball coated with petroleum jelly can help. They should gently pat the outer ear dry afterward or use a hair-dryer on a low, cool setting held at arm’s length. Reinforce the golden rule: no cotton buds or foreign objects in the canal. These remove protective wax and create micro-trauma that delays healing.
Pain control is often underestimated. Following the Therapeutic Guidelines: Pain and Analgesia, paracetamol or an NSAID should be recommended, provided there are no contraindications14. For children, provide clear weight-based dosing and encourage caregivers to track timing and response.
Topical therapy remains the foundation of management. The Therapeutic Guidelines: Antibiotic recommend antibacterial ear drops, with or without corticosteroids, for seven to ten days15.
For acute diffuse otitis externa (when fungal infection is not suspected), the recommendation is to use:
- ciprofloxacin +hydrocortisone 0.2% + 1% ear drops, twice daily for seven days
or
- dexamethasone + framycetin +gramicidin 0.05% + 0.5% + 0.005% ear drops three times daily for seven days.
These act directly where infection occurs and usually bring relief within two to three days.
Where the tympanic membrane is perforated or uncertain, pharmacists should recommend or ensure use of a non-ototoxic formulation e.g. ciprofloxacin. If there are signs of fungal OE such as persistent itch and characteristic debris, an antifungal, such as triamcinolone + neomycin + gramicidin + nystatin ear drops or flumetasone + clioquinol ear drops, may be required.
Correct technique is vital. Patients should warm the bottle in their hand, lie with the affected ear facing up, straighten the ear canal (up and back for adults, down and back for children), instil the prescribed number of drops without touching the dropper to the ear, gently press the tragus to help the liquid flow, and stay in that position for about five minutes16,17.
Most uncomplicated cases improve within 48–72 hours and resolve fully within two weeks18. If pain worsens, discharge persists beyond two weeks, or new systemic symptoms appear, they should seek medical review immediately. Clinical review is generally not required.
The final often overlooked step in every ear consult is prevention. Explain that recurrence is common but preventable. Encourage swimmers to tip and dry after water exposure, keep earphones and hearing aids clean and dry, and avoid inserting objects into the canal. For those with recurrent infections and intact eardrums, drying drops (acetic acid with isopropyl alcohol) after swimming can restore the ear’s natural pH and reduce bacterial growth15.
Case study
A 25-year-old presents with ear pain that has developed over the past two days. Her symptoms include a watery discharge after a weekend of swimming. There’s tenderness on tragal pressure and canal swelling, but no fever or systemic symptoms.
The pharmacist recognises uncomplicated AOE, explains the condition, provides analgesic advice, and prescribes topical therapy. She’s counselled on ear-drop use and strict keep-dry measures. Although there is generally no need to clinically review the patient, two days later she reports significant improvement, and a week later the infection has resolved. The follow-up conversation with her focuses on prevention, avoid cotton buds, dry the ear after swimming, and consider drying drops if infections recur.
These everyday cases illustrate why pharmacist involvement matters. Pharmacies are often the first and most accessible point of care. When pharmacists take a thorough history, perform focused observation, and apply structured reasoning, they can identify uncomplicated cases, manage symptoms safely, and recognise when referral is critical. Even without prescribing rights, pharmacists can deliver enormous value through assessment, education and preventive care.
Ultimately, managing swimmer’s ear well isn’t just about drops, it’s about dialogue. When pharmacists take the time to ask, look, think and teach, they transform a painful nuisance into a learning moment that prevents the next episode.
Australia
Competencies addressed: 1.5, 2.2, 2.3, 3.1, 3.2, 3.5
Accreditation Expires: 30/11/2027
Accreditation Number: A2512AUP2
This activity has been accredited for 0.75 hr of Group 1 CPD (or 0.75 CPD credit) suitable for inclusion in an individual pharmacist’s CPD plan which can be converted to 0.75 hr of Group 2 CPD (or 1.5 CPD credits) upon successful completion of relevant assessment activities.
New Zealand
This article aims to equip you with the tools necessary to meet recertification requirements and actively contribute to the growth of
your professional knowledge and skills.
Effectively contribute to your annual recertification by utilising this content to document diverse learning activities, regardless of whether this topic was included in your professional development plan.
References
- Rosenfeld RM, Schwartz SR, Cannon CR et al. Clinical practice guideline: Acute otitis externa. Otolaryngol Head Neck Surg. 2014;150(1 Suppl):S1–S24.
- StatPearls. Otitis Externa. Treasure Island (FL): StatPearls Publishing; updated 2025.
- American Academy of Family Physicians. Acute otitis externa: A practical guide to treatment and prevention. Am Fam Physician. 2001;63(5):927-36.
- DermNet NZ. Otitis externa – Overview and management. Accessed 2025.
- Perth Children’s Hospital. Otitis externa – ED guideline. Updated 2025.
- Janjulee E, Beyea JA, Simpson MTW et al. Approach to otitis externa. Can Fam Physician. 2013;59(12):e567-e572.
- Silverman J, Kurtz S, Draper J. Skills for Communicating with Patients. 3rd ed. CRC Press; 2013.
- Therapeutic Guidelines. Antibiotic– Ear, nose and throat infections: Otitis externa. Current edition.
- Remote Primary Health Care Manuals. Clinical Procedures Manual. 2025.
- Rosenfeld RM et al. AAO-HNSF guideline summary. Otolaryngol Head Neck Surg.2014;150(1 Suppl):S1–S24.
- Therapeutic Guidelines. Antibiotic – Acute external otitis management and referral criteria.
- Grandis JR et al. Necrotising otitis externa. N Engl J Med. 1992;327:1735-40.
- Therapeutic Guidelines. Antibiotic – Principles of topical therapy.
- Therapeutic Guidelines. Pain and Analgesi– Pharmacological management of acute pain.
- Australian Medicines Handbook. Ear infections; NSAIDs; Analgesics.2025 ed.
- ENT UK. How to use ear drops correctly. Patient information leaflet. 2024.
- NPS MedicineWise. Using ear drops safely and effectively. Accessed 2025.
- MSD Manual (Professional version).External otitis (acute): Overview. 2025.










