Patient savings from 60-day dispensing and co-payment reductions
In their Impact Analysis Report for the AUD25.00 copayment, Australia’s health department included a table which compared the patient savings from various medicine affordability measures introduced to the PBS since 2022 – including Safety Net threshold reductions, co-payment reductions and freezes, and 60-day dispensing.
The figures showed the January 2023 reduction in the general co-payment (from AUD42.50 to AUD30.00) had generated patient savings more than three times as much as 60-day dispensing.
Co-payment reductions have a much broader effect and achieve savings without introducing the potential for negative clinical outcomes or medicine wastage.
With the decision to reduce the maximum co-payment further to AUD25.00 from January 1, 2026, the Pharmacy Guild of Australia (PGA) predicts savings from the co-payment reductions, and the co-payment freeze introduced through the 8th Community Pharmacy Agreement (8CPA), will reach AUD1.6 billion by the end of 2026.
| Affordability measure | Prescriptions | Patient savings |
|---|---|---|
| 2022 Safety Net threshold reduction | 71,666,343 | $535,765,814 |
| 2023 general patient co-payment reduction | 59,937,171 | $758,299,154 |
| 2023 60-day dispensing | 34,371,235 | $247,204,792 |
| 2025 concessional patient co-payment indexation freeze | 77,294,748 | $11,215,939 |
| 2025 general patient co-payment indexation freeze | 12,509,884 | $15,458,394 |
Additional Community Supply Support (ACSS) payments
The government’s announcement of the introduction of 60-day prescriptions triggered a response from the community pharmacy sector and other stakeholders that ultimately resulted in the negotiation of the 8CPA one year earlier than scheduled.
Importantly, after recognition of the financial impact of the new policy, new ACSS payments were introduced as part of the 8CPA and enshrined in federal legislation. The ACSS payments are designed to financially support community pharmacies for dispensing PBS medicines, particularly those with increased dispensing quantities.
The ACSS payments include two parts:
Component 1 - an additional Administration, Handling and Infrastructure (AHI) fee for every 60-day prescription dispensed; and
Component 2 – a balancing amount that will ensure the AUD2,111 million in ACSS committed to under the 8CPA will be paid in full.
There is no direct offset for the loss of dispensing fees; however, the introduction of the ACSS payments is in recognition of the significant fixed costs involved in pharmacy operations, including the core function of dispensing.
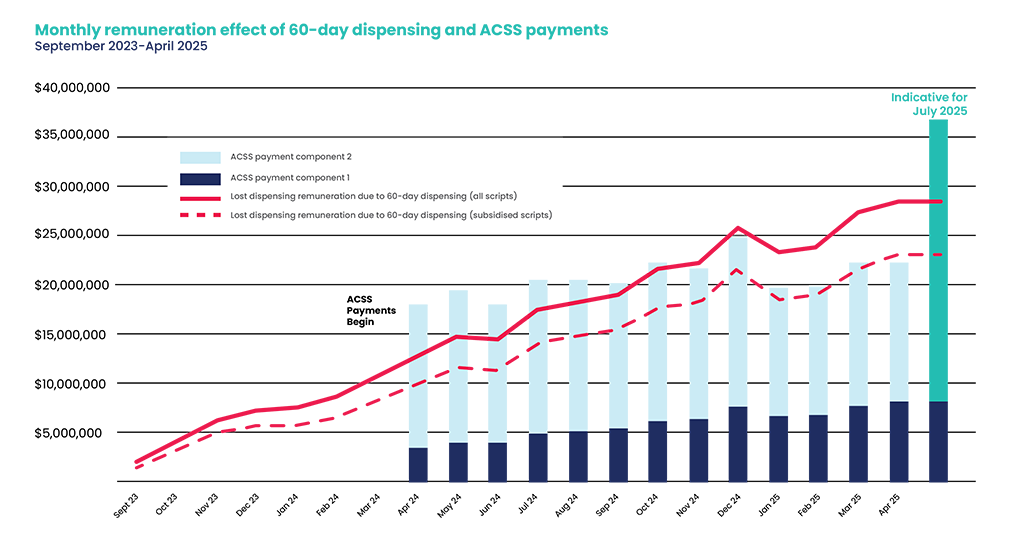
The chart below shows (in red) the month-by-month lost dispensing remuneration (dispensing fees and AHI fees) because of 60-day dispensing. The blue bars show the ACSS payments in comparison.
Crucially, the 8CPA includes a Payment Adjustment Mechanism (PAM) which ensures that the AUD2,111 million will be fully paid. This will be implemented through six-monthly adjustments to Component 2 of the ACSS payments.
Monthly remuneration effect of 60-day dispensing and ACSS payments
The first adjustment, applied from July 1 through to December 31, 2025, has resulted in an increase in that component from the initial level of AUD0.78 to AUD1.57 per subsidised prescription dispensed (both 30 and 60-day prescriptions).
Although July 2025 PBS data was not available at the time of writing, the last bar in the chart provides an indicative impact of this adjustment.
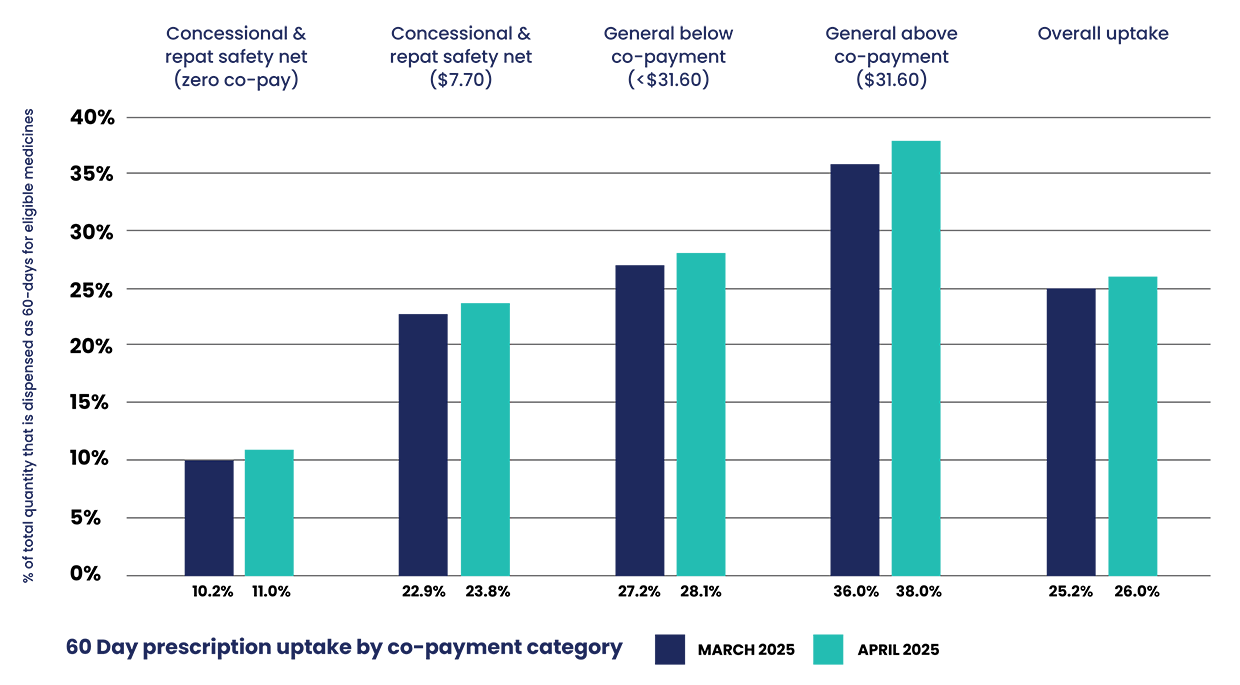
60-day uptake varies by co-pay level
Official PBS data through to April 2025 shows that the uptake rate of 60-day prescriptions varies widely, in line with co-payment levels. This may be partly due to the different levels of savings that accrue to the patient from 60-day scripts but also may be a sign of the different levels of complexity in medicine regimens.
For instance, concessional patients who frequently reach the safety net often manage complex medication regimens. Many prescribers may deem them unsuitable for longer dispensing durations, favouring more frequent pharmacist consultation and monitoring.
60-day prescription uptake by co-payment category - the New Zealand context
New Zealand readers will have read about Australia’s 60-day prescriptions and compared it to their own 90- day stat prescription duration, and discussions there about extending prescription duration to 180 days. There are, however, some crucial differences between the arrangements on either side of the Tasman.
Firstly, in Australia, the number of repeats and the dispensing frequency (typically one month until 60-day prescriptions, now often two months) is determined solely by the prescriber. The pharmacist has no ability to override the prescribed frequency.
In New Zealand, 90-day all-at-once dispensing is the default; however, registered Long-Term Conditions (LTC) patients can have their frequency of dispensing changed to any duration that their pharmacist deems appropriate to meet that LTC patient’s compliance and adherence needs1.
For non-LTC patients, pharmacists may authorise dispensing in monthly lots without prescriber authority. No such flexibility exists in Australia in relation to 60-day prescriptions. Patients may have their medicines periodically packed in dose administration aids (DAAs, “compliance packs” in New Zealand); however, there is no dispensing fee attached to this.
Secondly, Australians pay a co-payment for every dispensing, whether it is an original or a repeat (New Zealanders only pay for the original). This is how the patient saving is derived – essentially from a system that is already less affordable than the NZD5.00 maximum co-payment in New Zealand.
A new initiative was announced in New Zealand’s 2025 budget to extend the maximum prescription length from three months to twelve months. However, from an Australian perspective, it is important to understand what this means. It does not mean there will be 365 days of medicine dispensed all at once.
Medicines in New Zealand will continue to be dispensed at a maximum of three-month intervals. The announced change relates to the period of validity for a prescription before a new one is required from a GP.
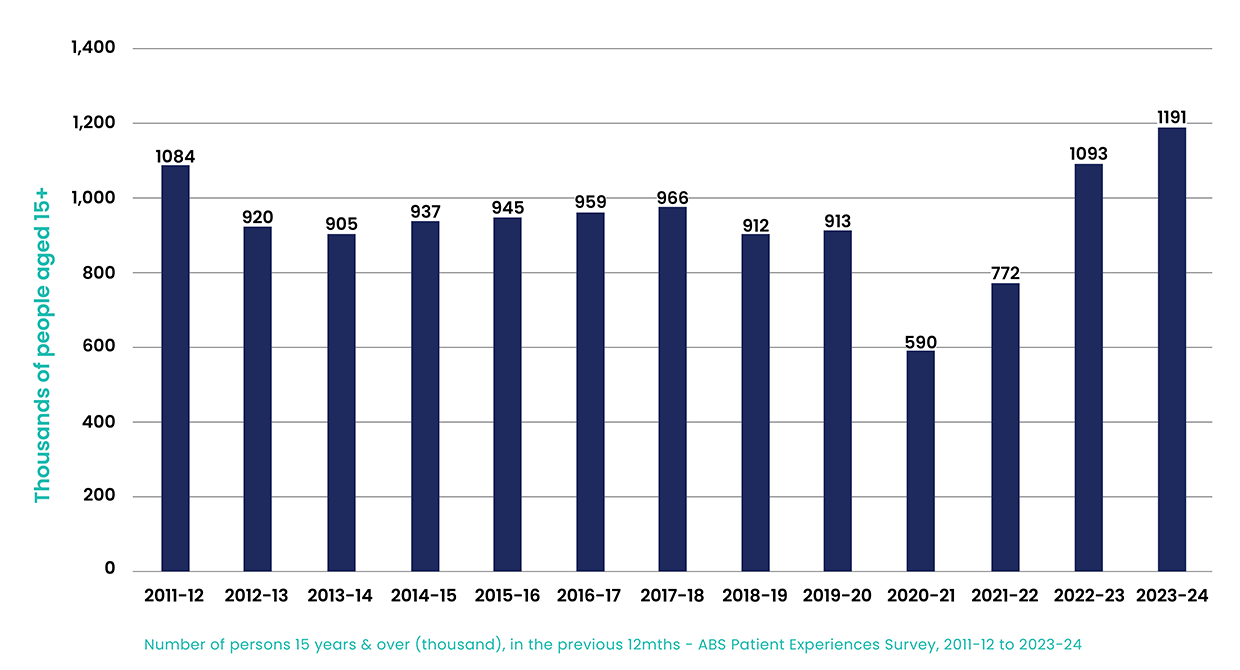
Co-payment reductions effectively improve medicine affordability
The latest data from the ABS in the chart below shows that medicine affordability continues to be a major problem in Australia, which is not surprising when our maximum copayment – even at AUD25.00 – sits near the highest in the developed world, many times higher than in New Zealand.
While 60-day prescriptions are here to stay, the evidence shows co-payment reductions are a far more effective way to improve medicine affordability, with the bonus of having the full support of the Australian public and the community pharmacy sector and not reducing the frequency of valuable patient encounters with health care professionals.
By reducing the emphasis on price, patient interactions with pharmacists can focus on optimising quality use of medicines. By continuing to prioritise direct affordability measures, we can ensure all Australians – regardless of their circumstances or which medicines they are prescribed – can access the medicines they need without financial hardship, through a highly accessible, thriving network of community pharmacies.
Equity of access is a key principle of our National Medicines Policy, and the Pharmacy Guild of Australia will continue to advocate on behalf of patients to make medicines more affordable.