Introduction
Clinical governance may be seen as the responsibility of an owner or manager of the pharmacy rather than an individual. While owners and managers do carry a higher burden of responsibility, clinical governance applies to all pharmacists. An understanding of these principles and how to apply them is essential to delivering best practice patient care.
In this article we will outline the topic in brief and provide a framework for pharmacists to consider for their own practice.
According to the Australian Commission on Safety and Quality in Health Care (ACSQHC), “clinical governance is the set of relationships and responsibilities established by a health service organisation between its state or territory department of health, governing body, executive, workforce, consumers and other stakeholders to ensure good clinical outcomes.”i
It applies to all stakeholders involved in the provision of health care services, from healthcare providers to managers, owners and governing bodies. It is recognised that in the smaller health care services these roles might be performed by the same individual.i
The Commission has developed a National Model Clinical Governance Framework based on the National Safety and Quality Health Services Standards, in particular the Clinical Governance Standards and Partnering with Consumers standard. i
The framework describes the systems and processes that are required to ensure the delivery of safe and effective health care, and which supports their implementation.ii
To help pharmacists contextualise the National Model Clinical Governance Framework, the Pharmaceutical Society of Australia (PSA) has developed Clinical Governance Principles for Pharmacy Services.iii These principles are intended as a guide for the design, implementation, and ongoing evaluation of pharmacy services, including Medication Management Review services.iii The following section outlines the five principles necessary to have good clinical governance and provides examples of how these relate to pharmacy services.
You should familiarise yourself with these and think about how you may implement them.
Principles of Clinical Governance

Partnering with consumers (patients)iii
The consumer’s needs and preferences must be considered. For the consumer to be an active participant in this process, communication should be at a level appropriate for the consumer’s health literacy. Pharmacists should actively seek feedback from consumers (ie. patients/referrers) and use it to drive quality improvement activities.
Governance, leadership and culture iii
Pharmacists should develop policies and processes that ensure safe, effective and sustainable healthcare, balancing workload
to allocate sufficient time for services. They should also ensure access to essential clinical resources. Promoting a culture of safety involves recognising the diversity of consumers and providing culturally appropriate and safe care. Additionally, pharmacists must maintain appropriate clinical expertise in identifying and managing clinical risks, monitor and improve service delivery systems and work collaboratively within multidisciplinary healthcare teams.
Clinical performance and effectiveness iii
Adherence to professional guidelines and standards to guide service delivery. Pharmacists should provide evidence-based care integrating the best available evidence with clinical experience and the consumer’s individual values and preferences. It is crucial to ensure that information provided to consumers about the service is transparent and that any incidents are disclosed to consumers and any other relevant stakeholders. Continual professional development is based on identified individual needs for the effective provision of pharmacy services. Furthermore, measuring, monitoring and reviewing the effectiveness of pharmacy services by undertaking audits should occur. These could include staff competency, inventory control and consumer or other stakeholder feedback.
Patient safety and quality improvement systems iii
Pharmacists identify safety risks and develop policies and procedures on how to minimise risk and manage incidents, such as by implementing a privacy policy. They adhere to relevant codes of practice, standards and legal requirements. They also implement a continuous cyclical quality improvement process, which includes periodic review of staff competency, regular collection and analysis of consumer feedback and regular self-assessment against required performance outcomes set by the Australian Pharmacy Council (APC) to identify learning needs.
Safe environment for delivery of care iii
Pharmacy services are usually delivered in the community pharmacy; hence pharmacists need to ensure that the area used for pharmacy services:
- allows for privacy and confidentiality,
- has adequate space and seating,
- is accessible to the consumer
- has access to required resources or materials
Pharmacists should also provide culturally safe care, which may include undertaking training in cultural awareness and safety, and reflecting on how different cultures and beliefs affect consumers’ perceptions of their health and wellbeing. It would also be beneficial to reflect on one’s personal attitudes and beliefs and how these can be a barrier to providing culturally safe care.
Pharmacists are accountable for the health care outcomes of their consumers and can follow the principles to implement a simple but effective clinical governance model which will help them drive continual improvement activities to ensure better outcomes for their consumers.
Quality Use of Medicines (QUM)
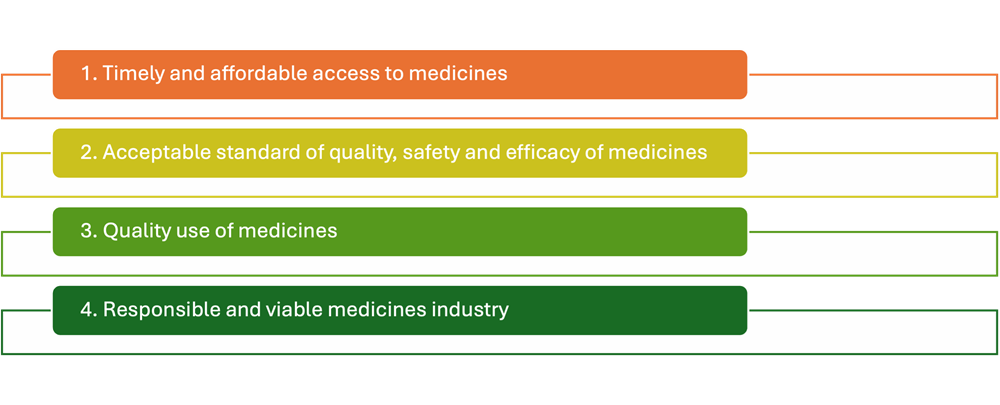
The Australian National Medicines Policy aims to ensure availability, affordability, quality, safety and efficacy of essential medicines in Australia.iv It has four main objectives:
Quality use of medicines (QUM) is defined as appropriate, judicious, safe and effective use of medicines:iv, v QUM can be achieved by:iv
- Selecting management options wisely in treating illness and maintaining health while recognising that non-pharmacological options may be more suitable to manage some disorders.
- When pharmacological treatment is considered necessary, choosing suitable medicines by considering:
- the individual and their beliefs and preferences
- the clinical condition
- risks and benefits
- dosage and length of treatment
- any co-existing conditions
- other therapies
- monitoring considerations
- costs for the individual, the community, and the health system
- Using medicines safely and effectively to get the best possible results by:
- defining goals of therapy and monitoring outcomes
- minimising misuse, over-use and under-use
- improving people’s ability to manage their medicines and any unwanted effects.
Pharmacists are committed to maintaining high professional standards and leveraging their expertise in medication management, guided by the principles of QUM. They acknowledge their responsibilities to both society and their profession. QUM principles are fundamental to pharmacists’ practice across all roles and settings.
The Commission collaborates with consumers, caregivers, healthcare professionals, and other stakeholders involved in delivery of health services to establish a safe, high-quality,
and sustainable healthcare system.vi Its key functions include developing national standards for safety and quality, crafting clinical care standards, coordinating efforts in specific areas
to enhance patient outcomes, and disseminating information, publications, and resources on safety and quality.vii
These standards include the National Safety and Quality Health Service Standards (which apply to hospitals, day procedure units and multipurpose health services and small hospitals) and National Safety and Quality Primary and Community Healthcare Standards which apply to delivery of care in primary and/or community settings.vii Adherence to these standards is crucial in addressing the safety and quality gaps that exist within Australia’s healthcare system. By implementing these standards, healthcare providers can ensure a consistent level of care across various settings, thereby reducing the incidence of avoidable negative events and improving overall patient outcomes.
Safety of consumers and workers in health care settings in Australia
While Australia's healthcare system generally produces positive results, there are instances where consumers don't receive the most suitable care, leading to avoidable negative events.viii Safety and quality gaps, along with inconsistencies in healthcare across different demographics in Australia, result in significant human and financial tolls.ix
Much of the research into patient safety to date has focused on the hospital setting where a large number of harmful but preventable incidents occur.ix These include health care-associated infections, hospital-acquired complications (including medication errors) and potentially preventable hospitalisations.ix
However, even though most health care is being provided in the primary health care setting, there is a lack of data on patient safety in this sector.ix Most of the available data focuses on voluntary reporting of errors and incidents.
In their 2010 draft report on patient safety in primary health care, the ACSQHC identified medication-related errors as a significant safety risk to consumers in the community.x
The most common contributing factor to medication related errors was found to be lack of communication between health professionals and consumers, between GPs and pharmacists and at transitions of care.x
The significant risk that medications pose to safety of consumers in Australia is evident from the data reported
in the PSA's Medicine Safety: Take Care report:x
- A quarter of a million people are hospitalised each year because of medication error, misuse and misadventure, at a cost of $1.4 billion.
- 400,000 presentations to emergency departments are likely to be due to medication-related problems.
- It is estimated that 50% of medication related harm is preventable.
- Over 90% of consumers have at least one medication-related problem post hospital admission
- 20% of people are suffering an adverse medication reaction at the time they receive a Home Medicines Review.
- 2 million Australians have experienced an adverse medication event in the last 6 months.
The Australian Commission on Safety and Quality in Health Care has come up with a plan to minimise medication harm related to three main areas of concern:xi
- Polypharmacy
- High-Risk Medicines
- Transitions of Care.
Safety of health care workers
Safe Work Australia outlines the common hazards and risks health care workers face and specifies the persons responsible for managing these risks.xii These include:xiii
- manual handling,
- biological and chemical hazards,
- workplace violence, bullying and harassment,
- mental health issues resulting from work related stress,
- fatigue,
- slips, trips and falls.
Privacy, confidentiality and consent in pharmacy services
Although used interchangeably, privacy and confidentiality are not the same thing. Privacy, in its legal context, goes beyond the issues of disclosure of personal information and covers issues of a patient's access to their own medical records, as well as security and maintenance of their records.xiii Privacy only relates to the personal identifiable information, whereas confidentiality relates to all information provided by the person to their health practitioner.xiv
Privacy and confidentiality are fundamental to good relationships between health care providers and consumers which goes
back to the Hippocratic Oath.xiv Without assurances that the information disclosed during the provision of a health service
is treated with confidentiality, consumers might be less likely to have frank conversations with their health care providers, which would ultimately lead to less-than-optimal care.xiv Health care providers, including pharmacists, need to safeguard this privilege by ensuring that they follow the Australian Privacy Principles (APPs) as set out by the Commonwealth Privacy Act and Commonwealth Privacy Amendment.xiv In addition to the negative impact on relationships, privacy breaches can incur penalties.xv
It is the responsibility of all pharmacists to be aware of the APPs and to ensure that they have policies and processes in place to safeguard the privacy of their consumers.xv The Pharmacy Guild of Australia and the PSA have jointly published a document titled Privacy and Pharmacy: What does it mean for you.xv This document is a summary of the APPs and whilst it does not cover every aspect of privacy law, it is a good starting point for pharmacists to familiarise themselves with their obligations. It also provides templates for:xv
- Privacy policy
- Complaint form
- Collection and disclosure of information
- Request for access
- Confidentiality undertaking
Australia
Competency standards addressed: 1.1, 1.2, 1.3, 1.4, 1.6, 2.1, 2.3, 3.1, 3.2, 4.7
Acceditation Number: 02507AUPI
Expires: 30/6/2027
This activity has been accredited for 0.75 hr of Group 1 CPD (or 0.75 CPD credit) suitable for inclusion in an individual pharmacist’s CPD plan which can be converted to 0.75 hr of Group 2 CPD (or 1.5 CPD credits) upon successful completion of relevant assessment activities.
Authors: Mirna Sydenham BPharm MClinPharm and Georgette Yassa BPharm MPS CredPharm (MMR)
New Zealand
This article aims to equip you with the tools necessary to meet recertification requirements and actively contribute to the growth of your professional knowledge and skills.
Effectively contribute to your annual recertification by utilising this content to document diverse learning activities, regardless of whether this topic was included in your professional development plan.










